Table of Contents
Introduction
Have you ever come across the term endometrial thickness? If you’ve been delving into women’s reproductive health or are trying to conceive, chances are, you have. But what exactly is it, and why is it so crucial for women?
What is Endometrial Thickness?
The endometrium is the innermost lining of the uterus. Its thickness, or the ‘endometrial thickness’, is a crucial parameter in various reproductive processes and diagnostics. It’s like the soil in a garden – you need the right depth and quality for plants to grow.
Why is it Important?
A healthy endometrial lining ensures optimal conditions for implantation of a fertilized egg. Think of it as the comfortable bed where the embryo snuggles in to grow.
Understanding Endometrial Thickness
Now, let’s dive deeper and understand the ranges of endometrial thickness and how it varies.
Normal Endometrial Thickness: What’s the Range?
In general, a normal endometrial thickness is between 8-11mm during a woman’s reproductive years. However, just like how people have different heights and builds, there’s some variation in what’s considered ‘normal’.
Variations through the Menstrual Cycle
Ever wondered if the endometrial lining remains static throughout the month? It doesn’t. Its thickness varies across the menstrual cycle, being the thinnest post-period and the thickest just before menstruation begins again.
Role of Endometrial Thickness in Reproduction
Embryo Implantation
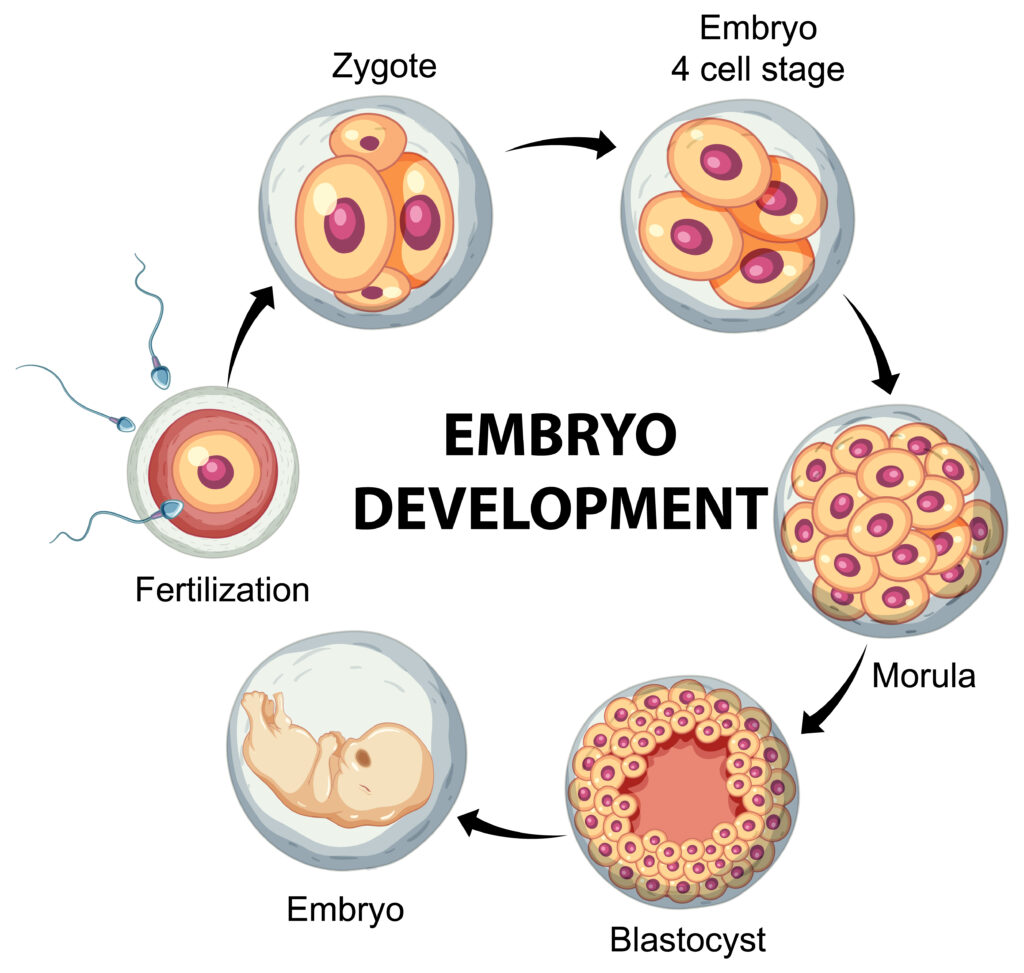
The endometrium’s main role is to provide a nurturing environment for a fertilized egg, known as an embryo. After successful fertilization, the embryo starts its journey down the fallopian tube towards the uterus. If the endometrial lining is receptive and adequately developed, the embryo can implant itself into the uterine wall. However, if the endometrium is not in an optimal state, the embryo may fail to implant, resulting in a failed pregnancy.
Nutrient Supply

Once the embryo implants, the endometrial lining continues to play a vital role by supplying essential nutrients and oxygen to the developing embryo. This ensures the embryo’s proper growth and development during the early stages of pregnancy.
Hormonal Support
The endometrium also produces various hormones and growth factors that are crucial for maintaining pregnancy. These substances support the corpus luteum—a temporary endocrine structure formed after ovulation—ensuring a steady supply of hormones that are necessary for the first trimester of pregnancy.
Thin Endometrium causes
Various factors can leave this fertile ground less than ideal. Here’s a look at some of the primary culprits:
Hormonal Imbalances
Just like how a plant needs the right amount of sunlight and water to thrive, our endometrium requires a balanced cocktail of hormones. Thin endometrium causes often root back to imbalances in estrogen, which is essential for endometrial growth
Estrogen Deficiency
Estrogen, a crucial hormone for women, aids in building the endometrial lining. Think of it as the water and sunshine needed for plants to grow. Without adequate estrogen, the endometrial lining might not thicken adequately.
Thyroid Dysfunction
Did you know that your thyroid can affect your endometrial lining? An underactive or overactive thyroid can result in hormonal disturbances, including those that affect the uterus.
Poor Blood Circulation
Adequate blood circulation is crucial for delivering essential nutrients and oxygen to the endometrial tissue. Poor circulation can lead to insufficient nourishment, are some of the important thin endometrium causes.
Lifestyle and Environmental Factors

Think of the endometrium as a sponge. Just as a sponge can dry out in harsh conditions, our lifestyle and environment can affect the health of our endometrium. Factors like smoking, low body weight, and excessive exercise can all be potential thin endometrium causes
Nutritional Deficiencies
A balanced diet is vital for overall health, including reproductive health. Nutritional deficiencies, especially of vitamins and minerals like vitamin E and omega-3 fatty acids, can impact endometrial thickness.
Surgical Procedures
Surgeries, especially those on the uterus like a D&C (Dilation and Curettage), can sometimes lead to scarring or Asherman’s syndrome, which can thin the endometrium. It’s like when land becomes barren after excessive farming.
Excessive Exercise

While regular exercise is beneficial, excessive and intense workouts can sometimes lead to hormonal imbalances that affect endometrial thickness
Prolonged Use of Certain Medications

Some medications, especially those related to cancer treatments or particular hormonal treatments, can affect the thickness of the endometrial lining. Always a good reason to keep track of what we’re putting into our bodies, right?
Thin Endometrium symptoms
Recognizing the symptoms is the first step towards addressing any health concern. Let’s delve into the specific thin endometrium symptoms.
Menstrual Irregularities

One of the primary thin endometrium symptoms is irregular menstrual cycles. If you’re missing periods or they’re coming too frequently, it might be a red flag.
Spotting Between Periods
Noticing a few drops here and there when it’s not that time of the month? This spotting can be a telltale sign of a thin endometrium.
Lighter Period Flow
One of the most evident thin endometrium symptoms is a notably lighter flow during periods. Instead of the usual 4-7 days, you might experience a shorter duration.
Difficulty in Conceiving
Faced with fertility challenges? A thin endometrial lining can make it difficult for an embryo to implant, leading to challenges in conception.
Chronic Pelvic Pain
While it can be associated with various conditions, consistent pelvic pain can also be a symptom of a thin endometrium.
Recurrent Miscarriages
While heartbreaking, recurrent miscarriages might be indicative of a thin endometrium.
Pain and Discomfort
While pain can stem from various factors, persistent pelvic discomfort may be linked to a thinning endometrial lining.
Treatment Options for Thin Endometrium Lines
So, what can be done if you’re diagnosed with a thin endometrial lining? Let’s explore some thin endometrium treatment options.
Increased Blood Flow Improving blood flow can work wonders for your endometrial lining.
Acupuncture This age-old treatment can stimulate blood flow to the reproductive organs.
Physical Therapy Specific exercises can boost circulation to the pelvic region, aiding in endometrial growth.
Hormonal Therapies Sometimes, the body needs a little hormonal nudge.
Estrogen Therapy Oral or vaginal estrogen can help in thickening the endometrial lining.
Vitamin E and L-arginine These supplements are believed to enhance endometrial thickness by improving blood flow.
G-CSF Therapy Granulocyte colony-stimulating factor can be used to enhance endometrial growth.
PRP (Platelet-Rich Plasma) Injections Recent studies have shown promising results in enhancing endometrial growth using PRP injections.
Stem Cell Therapy This cutting-edge thin endometrium treatment involves injecting stem cells into the endometrium to rejuvenate and regenerate it.
Uterine Scratching A slightly abrasive procedure, it’s believed to trigger the body’s healing response, resulting in a thicker endometrial lining.
Natural Remedies Sometimes, nature holds the answers.
Diet and Lifestyle Changes Foods rich in omega-3 fatty acids and antioxidants can aid in thickening the endometrial lining. Regular exercise, managing stress, and avoiding toxins can also help.
When to Seek Medical Help If you’ve been trying to conceive for a while or suspect an issue with your endometrial lining, it’s essential to consult a healthcare professional. They can provide guidance on the best thin endometrium treatment for you.
What is Endometrial Cancer?
Have you ever heard of endometrial cancer? This type of cancer begins in the lining of the uterus, known as the endometrium. It’s one of the most common cancers in the female reproductive system. But don’t let that scare you – understanding it is half the battle.
Causes and Risk Factors
So, what causes endometrial cancer? While the exact cause is unknown, several factors may increase the risk, including age, hormone therapy for breast cancer, or a history of endometrial polyps. Remember, risk factors don’t guarantee you’ll get the disease, but being aware is crucial.
Steps in Endometrial Cancer Diagnosis
Symptoms Indicating a Need for Diagnosis
If endometrial cancer were a burglar, what signs would show us it’s lurking? Vaginal bleeding after menopause, pain during sex, and pelvic pains are its footprints. Recognizing these signs is like setting up an alarm system – it helps you act quickly.
Diagnostic Tests
You might wonder, “how do doctors confirm the presence of this unwelcome intruder?”
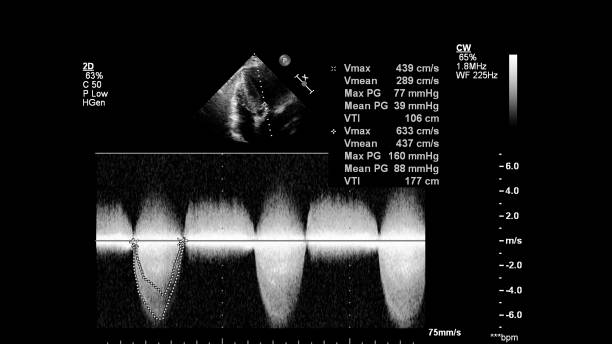
Ultrasound
Think of an ultrasound as the security camera of the medical world. It uses sound waves to capture images of the inside of the uterus, checking for any unusual growths.
Biopsy
A biopsy is like catching a suspect red-handed. It involves taking a small sample of the endometrial tissue to examine for cancer cells.
MRI
An MRI scan? It’s like having a detective on the case, providing a detailed image of the uterus to find hidden traces of the disease.
The Importance of Early Diagnosis
Why Time is of the Essence
You’ve probably heard that time flies, right? Well, when it comes to endometrial cancer diagnosis, time truly is of the essence. Early diagnosis means more treatment options and better chances of recovery.
Potential Outcomes of Late Diagnosis
Delay is dangerous! Late diagnosis could lead to the cancer spreading to other parts of the body, making treatment more challenging. It’s like realizing your house has been leaking only after the floor is flooded.
Treatment Options Post-Diagnosis
Surgical Approaches
Think of surgery as evicting the unwanted intruder. It often involves removing the uterus, fallopian tubes, and ovaries.
Radiation and Chemotherapy
Imagine these treatments as the security reinforcements post-burglary. They aim to kill or shrink cancer cells and prevent them from coming back.
Conclusion
Endometrial thickness plays a pivotal role in women’s reproductive health. While a thin endometrial lining poses challenges, with the right knowledge and timely intervention, many women can navigate these hurdles. It’s all about understanding the soil of your garden and ensuring it’s ripe for growth.
FAQs
What is the ideal range for endometrial thickness?
Typically, a thickness of 8-11mm is considered normal during a woman's reproductive years.
Can I naturally improve my endometrial thickness?
Yes, lifestyle changes like a balanced diet, regular exercise, and quitting smoking can help improve endometrial thickness.
Does a thin endometrium always mean fertility issues?
Not always, but it can reduce the chances of embryo implantation. However, every individual is different, and it's best to consult with a healthcare professional.
Are there surgical options to treat thin endometrial lines?
Yes, certain surgical methods can help treat thin endometrium, depending on the cause.
Is age a significant factor affecting endometrial thickness?
Age can play a role in endometrial thickness, with the lining often becoming thinner as a woman ages.

